Clinics in National Skin Centre
Patients with special needs are subsequently referred to subspecialty clinics. Patients are seen at our general clinics first before they can be referred to the subspecialty clinic.
NSC has the following subspecialty clinics:
Acne Clinic
Consultant-in-charge: Adj A/ Prof Hazel Oon
The Acne Clinic was started in May 2009, and operates on Tuesday afternoons.
Acne vulgaris is the second most common new condition seen at NSC. It can be associated with significant morbidity, such as scarring and keloid development, especially in patients with severe, inflammatory lesions. These patients may require oral medication in addition to topical medication for management of acne, and are closely monitored and cared for by our team of doctors and nurses in this clinic. Handling psychosocial stress of acne patients is another important aspect of patient care and the Acne Clinic works in collaboration with the Skin Health Clinic on this issue.
Objectives of the Clinic
- To allow research in areas of epidemiological data analysis, microbiological research pertaining to acne pathogenesis, clinical outcomes and longitudinal follow-up.
- To provide comprehensive and quality care for patients (including adults and teenagers) with moderate to severe acne vulgaris.
Cases for referral to Acne Clinic
- Any teenage or adult patient with moderate to severe inflammatory acne vulgaris and nodulocystic acne. This includes treatment-naïve patients and patients already on topical and or systemic therapy for acne. In particular, all patients on oral isotretinoin therapy for acne should be referred to this clinic for further follow up and management.


Acne
Contact Dermatitis and Joint Occupational Dermatoses Unit
Chief: Adj A/ Prof Leow Yung Hian, , Advisor: Dr Anthony Goon
The Contact Dermatitis Clinic evaluates and investigates patients who present with dermatitis that may have a suspected exogenous cause. Special investigations, like patch testing and prick testing, are performed in this clinic.
The Joint Occupational Dermatoses Clinic manages patients where the cause of exogenous dermatitis is thought to be occupationally related. It is a collaboration between the National Skin Centre and the Occupational Health Department, Ministry of Manpower. It convenes fortnightly and screens through patients from both the General Clinics of National Skin Centre and referrals from occupational physicians or private practitioners. Specific recommendations for the patients are made after complete evaluation and investigation at the clinic. Invenstigation includes patch testing, prick testing and sometimes, factory visits.

Patch Testing
Cutaneous Infection Unit
Chief: Adj A/Prof Pan Jiun Yit, Deputy: Dr Kuan Ling Yee
The Cutaneous Infection Unit attends to patients with skin infections particularly leprosy, cutaneous TB, MOTT infections, chromoblastomycosis, sporotrichosis, mycetoma, recalcitrant tinea corporis, tinea versicolor and onychomycosis. The unit also manages cutaneous infections in immunocornpromised patients, including those with HIV infection and organ transplant recipients. It also undertakes to ascertain the causes of granulomas, especially infective granulomas.
Dermatological and Laser Surgery Unit
Chief: Dr Suzanne Cheng
Mandalay Clinic (MAC) Laser Suites provide a comprehensive range of procedural dermatological services. The facility houses 4 consultation rooms, 6 laser suites with adjoining recovery rooms, 2 nurse counselling rooms and a photography room. The entire facility was meticulously designed to ensure smooth workflow and provide patients with maximal privacy in an elegant setting.
MAC is equipped with a comprehensive range of dermatological lasers. These include the Smartxide 2 fractional TM carbon dioxide laser, Revlite TM pigment laser, V-Beam Perfecta TM vascular laser, Ellipse PPT TM intense pulsed light device, Long-pulsed Nd:YAG laser (for hair removal), 1450nm non-ablative diode laser (for skin rejuvenation) and DermaRF TM skin tightening device. MAC is currently a one-stop laser centre for the treatment of a wide range of cosmetic skin problems including birthmarks, skin pigmentation, wrinkles, acne scars, benign skin growths, broken veins and sagging skin.
Adjoining MAC is the Procedure Suites housing 4 surgical rooms for the management of skin cancers and other non-cosmetic skin conditions. The facility is fully equipped to perform Mohs micrographic surgery, a specialised surgical technique which allows skin cancers to be removed with maximal preservation of uninvolved tissue and is associated with the highest cure rates.

Laser in use at the Operating Theatre
Clinical Indicator:
Infection Rates of Procedures
Dermatopathology Division
Chief: Adj A/Prof Joyce Lee Siong See, Deputy: Dr Tee Shang Ian
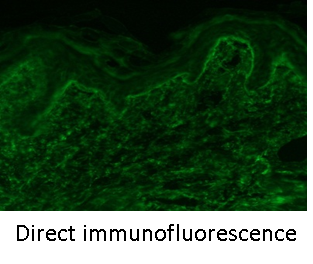
The division provides timely and accurate pathologic diagnoses spanning the wide spectrum of skin diseases, ranging from common conditions, to rare and complex ones. This is made possible by a team of in-house, certified and dedicated dermatopathologists who work closely with clinicians in NSC and referring physicians, both locally and internationally. Through histopathology, coupled with use of immunohistochemistry and direct immunofluorescence techniques, precise reports are provided to facilitate treatment.
Drug Eruption Clinic
Consultant-in-charge: Adj A/Prof Lim Yen Loo, Deputy: Dr Lucinda Tan
The Drug Eruption Clinic attends to patients who are referred for evaluation and management of possible or confirmed drug-induced adverse skin reactions. Apart from detailed reviews of patients' presenting histories and physical findings, investigations such as drug-specific IgE tests, skin prick tests, intradermal tests and patch tests will be offered to patients, if relevant. Drug provocation tests are also performed in this clinic, when indicated.
This clinic operates on the first and third Mondays of every month.
Laser in use at the Operating Theatre
Eczema Clinic
Consultant-in-charge: Dr Yew Yik Weng
The Eczema Clinic was started in August 2008. It operates every Monday afternoon, and it aims to provide comprehensive and quality care for adult patients with moderate-to-severe atopic eczema or other forms of endogenous eczema.
Patients who require systemic immunomodulatory drugs for eczema will be cared for by a team of doctors and nurses with special interest in the area. There will also be specialized patient counseling / education. The Eczema Clinic will function in close collaboration with the other subspecialty clinics, including Paediatric Dermatology Clinic, Contact Clinic, Photobiology Clinic and Skin Health Clinic.

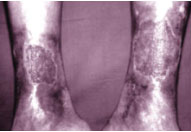
Eczema
Clinical Indicator :
Percentage of patients with at least 25% improvement in POEM
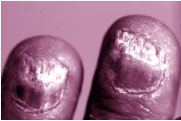
Hair and Nail Clinic
Consultant-in-charge: Dr Etienne Wang, Advisor: Adj A/Prof Joyce Lee Siong See
The Hair and Nail Clinic offers skilled management of hair, scalp and nail disorders. All aspects of hair loss and nail disorders are managed here. Research projects on the treatment and pathogenesis of hair loss as well as a comprehensive teaching programme, are also conducted in this clinic.

Immunodermatology Unit
Chief: Adj A/Prof Lim Yen Loo, Deputy: Dr Heng Yee Kiat
The Immunodermatology Unit focuses on the evaluation and management of patients with immune-mediated skin conditions, which may require the use of immunosuppressive drugs.
Examples of skin conditions managed in this Unit include:
- Immunoblistering diseases: bullous pemphigoid, pemphigus, linear IgA bullous dermatosis, dermatitis herpetiformis, paraneoplastic pemphigus
- Connective tissue diseases: cutaneous lupus erythematosus, dermatomyositis, morphoea, scleroderma
- Cutaneous vasculitis
- Others: Behcet's disease, Sweet's syndrome, recurrent erythema multiforme, pyoderma gangrenosum, livedoid vasculopathy
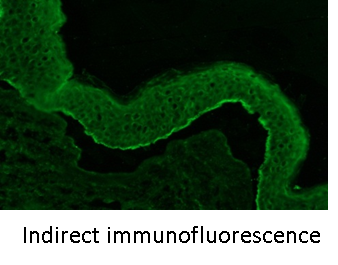
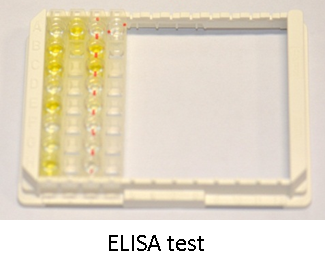
Patients will undergo detailed clinical evaluation and appropriate skin and laboratory investigations at this clinic. Available investigations include skin histopathology, direct and indirect immunofluorescence, anti-BP180 and anti-BP230 IgG ELISA tests, anti-desmoglein 1 and 3 ELISA tests, autoimmune serologies and immunoblot studies.

Clinical Indicator:
Monitoring of side effects in patients receiving systemic corticosteroid therapy
Inpatient Dermatology Unit
Chief: Dr Heng Yee Kiat, Deputy: Dr Wang Ding Yuan
The arm of Inpatient Dermatology at the National Skin Centre primarily serves the skin needs of patients admitted to Tan Tock Seng Hospital, Renci Community Hospital and the National Centre for Infectious Diseases.
We have 2 models of care in Inpatient Dermatology:
- Patients of NSC with poorly controlled or extensive skin disease may be hospitalised for the treatment of their skin condition. The Inpatient Dermatology team will be directly in-charge of the care of such patients upon admission. Common diagnoses encountered include Erythroderma, generalised Eczema or Psoriasis, Bullous Pemphigoid or Pemphigus.
- Patients hospitalised in the aforementioned hospitals under the care of other disciplines may be referred to the team of Inpatient Dermatologists for various skin disorders. Such referrals encompass a vast spectrum of skin diseases ranging from various fungal or scabetic infestations to cutaneous adverse drug reactions to other systemic illnesses and/or connective tissue diseases which manifest on the skin.
Itch Clinic
Consultant-in-charge: A/Prof Tey Hong Liang
Itch is the major source of morbidity in patients attending our clinics. Patients with severe and intractable itch are referred by dermatologists to the Itch Clinic. We aim to improve treatment of our patients suffering from severe and chronic itch through a holistic approach.
Scope
The scope of management of the clinic consists of the following conditions:
- Itch involving the whole body that is not due to an apparent underlying skin problem
- Itch involving a particular area of the body that is not due to an underlying skin problem
- Severe and chronic itch that is not responsive to treatment
Setup
The clinic runs weekly on Friday afternoons and takes referrals from dermatologists. It is located at Clinic H on the second floor of the National Skin Centre.

Multiple scratch-induced lesions on the back of a patient with severe itch involving the whole body.
Clinical Indicator:
Mean percentage reduction in itch score between the first and final visit
Lymphoma Clinic
Consultant-in-charge: Dr Tee Shang-Ian, Advisor: Prof Tan Suat Hoon
At the Lymphoma Clinic, a spectrum of cutaneous lymphomas is seen and managed. This comprises mycosis fungoides, Sezary syndrome, lymphomatoid papulosis, subcutaneous panniculitis-like T-cell lymphoma, other cutaneous T-cell and B-cell lymphomas.
Full clinical evaluation, review of histology in close consultation with the pathologist, and staging investigations are carried out. For complex cases, joint management with a multi-disciplinary team of radiation and medical oncologists is organized for optimal clinical care.
Paediatric Dermatology Clinic
Chief: Dr Lucinda Tan, Advisor: Dr Madeline Ho
The Paediatric Dermatology Clinic manages both common and difficult to manage skin disorders cases in infants and children, including genodermatoses, metabolic disorders and infections. The physical set-up will include consultation clinics, procedure/ treatment and testing rooms, nurse educator and counseling room with resource materials. With the comprehensive care and management, this clinic will be able to help more children with skin disorders achieve a higher quality of life.

Parents are guided at hands-on therapy sessions
Pigment Clinic
Consultant-in-charge: Adj Prof Steven Thng
The Pigment Clinic is held once a week. Patients with pigmentation problems are referred to the clinic for evaluation and management. Various treatment modalities, including topical medications, various forms of phototherapy (including topical and systemic PUVA, narrowband UVB, excimer laser) and various surgical procedures (including minigrafting and suction grafting) are used to treat our patients. In addition, the clinic is also actively involved in various research projects on Vitiligo, such as setting up of the Melanocyte Culture Laboratory and exploring the possibility of autologous melanocytes transplant.
Photodermatology Unit
Chief: Dr Eugene Tan, Advisor: Adj A/Prof Chong Wei Sheng
The Photodermatology Unit attends to patients with photodermatoses or "sun allergy". Patients are evaluated based on their medical history, physical examination, phototesting and laboratory investigations. Dermatological conditions treated with various phototherapy or "light therapy" modalities include psoriasis, mycosis fungoides, vitiligo, atopic dermatitis, pityriasis lichenoides, eczema of the hands and feet, morphoea, uraemic pruritus, acne and skin cancer.
The Phototherapy division of the Photodermatology Unit provides the following phototherapeutic modalities :
- Narrowband UVB phototherapy
- UVA/Narrowband UVB combined phototherapy
-
Systemic PUVA photochemotherapy
- Bath PUVA photochemotherapy
- Soak PUVA photochemotherapy
- Paint PUVA phototherapy
- UVA1 phototherapy
- Excimer lamp targeted phototherapy
- Photodynamic therapy
- Omnilux Blue phototherapy
The Photodiagnostic division of the Photodermatology Unit provides the following diagnostic methods:
- Phototesting
- Photoprovocation testing
- Photopatch testing
- Systemic Drug Photochallenge
In phototherapy and photochemotherapy, both UVA and UVB may be used in combination with oral medications such as Acitretin (a retinoid or Vitamin A medication) and Methotrexate. Combination treatments increase the effectiveness in clearing psoriasis. ReNBUVB refers to the combined use of Acitretin and narrowband UVB phototherapy. Similarly, RePUVA is the combination therapy of Acitretin and PUVA photochemotherapy. These 2 combination modalities are very effective for the treatment of generalised and severe plaque psoriasis. They are generally recommended for those who fail to respond to NBUVB and PUVA alone. Acitretin enhances the therapeutic effects of NBUVB and PUVA and reduces the number of phototherapy treatment sessions and the cumulative UV doses.
Photodynamic Therapy
Photodynamic therapy (PDT) involves the use of a photosensitiser and an activating light source in the treatment of skin diseases such as skin cancer. It was only with the development of topical PDT that its use in dermatology dramatically increased. In topical PDT, ALA (aminolaevulinic acid) or methylALA is applied onto the target skin lesion. This is taken up by the abnormal cells and converted to protoporphyrin IX via the haem biosynthesis pathway present within the cells. Protoporphyrin IX is a potent photosensitiser. It is activated by irradiation with an appropriate light source such as red light, resulting in generation of reactive oxygen species and damage to the target tissue. This treatment has been shown to be effective in skin diseases such as actinic keratosis, Bowen disease, superficial and nodular basal cell carcinoma. It has also been used in other dermatological diseases such as mycosis fungoides, viral wart, extramammary Paget disease, acne and keloid.
At NSC, we utilise the methylALA-Aktilite PDT system. This system is used commonly in Europe and Australia and we are the first institution in Asia to offer this treatment. It is a safe procedure with the main side effects of pain during the irradiation and possible redness and crusting, lasting up to a week after treatment. The procedure is simple. Topical methylALA or Metvix cream is applied to the lesion and left under occlusion for 3 hours. This is followed by irradiation with the Aktilite lamp (red light source) for about 8 min. Usually, 2 treatments a week apart are needed to treat actinic keratosis, Bowens disease and basal cell carcinoma. The advantage of this treatment is that it is a simple, non-invasive treatment with excellent cosmetic outcome and offers a good alternative treatment to traditional surgery. While it does not replace surgery in the treatment of Bowen disease and basal cell carcinoma, it offers an alternative to patients who are unsuitable or not keen on surgery and is a good option for treatment of lesions on difficult sites such as the face and ear or when a good cosmetic outcome is of great concern.
Excimer Lamp Targeted Phototherapy
From 1 September 2009, the National Skin Centre became the first healthcare institution in Singapore to offer the state-of-the art VTRAC excimer lamp phototherapy service to patients.
The excimer lamp source emits UVB light at a wavelength of 308 nm. This has been proven to be effective for a number of skin conditions, in particular psoriasis and vitiligo. It has been shown to clear psoriasis plaques faster with fewer treatments as compared to using NBUVB, and it is effective for vitiligo with repigmentation noted within weeks of treatment. The excimer lamp, which allows for targeted treatment of affected areas, complements the existing wide range of phototherapy devices already available at NSC. These devices include the NBUVB and UVA full-body cabins and the localised hand and feet PUVA systems.
Omnilux Blue Phototherapy
This system emits blue light at a wavelength of 415 nm, targeting the bacteria in the hair follicles called Propionibacterium acnes and killing them, thereby resulting in improvement of acne lesions. This system is used in the treatment of mild to moderate acne. Each treatment session lasts 20 min and the patient needs to come twice per week for the blue light therapy. It will benefit many patients with acne vulgaris where oral treatment is contraindicated or intolerant, or when one is not keen on oral therapy. This service will commence in the first quarter of 2016.
Psoriasis Unit
Chief: Adj A/ Prof Hazel Oon, Advisor: Adj A/Prof Chong Wei Sheng
The Psoriasis Unit attends to psoriasis patients - particularly those with severe disease. Modalities of treatment used include topical coal tar, dithranol, calcipotriol and topical steroids. Patients who require phototherapy are sent to the Phototherapy Unit for further management. Systemic therapy used include MTX, retinoids, ciclosporin and others.
The unit is actively involved in research in Psoriasis. The spectrum of research activities include clinical trials, epidemiological studies and basic research on psoriasis.
The unit also works with the Psoriasis Association of Singapore (PAS), a self-help support group.

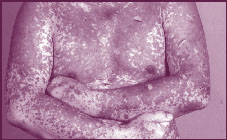
Phototherapy Treatment
Clinical Indicator:
Percentage of newly-diagnosed psoriasis patients started treatment in Psoriasis Clinic achieving at least 50% improvement in PASI
Screening Psoriasis patients for diabetic symptoms
Skin Health Clinic
Consultant-in-charge: Dr Su Pei Qi
This combined clinic manned by the psychiatrist and dermatologist manages chronic skin problems with psychosocial problems of anxiety and depression. Other psychoses managed include obsessive compulsive disorders, parasitophobia, dermatitis artefacta and trichotillomania. Residents are taught the psychoderm approach, psychopharmacology and techniques like behaviour change techniques, relaxation techniques and stress management. Many of our patients, who refused to go to the Pychiatric Unit are now managed here.
Skin Cancer Clinic
Consultant-in-charge: Dr Chia Hui Yi, Deputy: Dr Suzanne Cheng
The Skin Cancer Clinic serves to provide expert care for patients diagnosed with skin cancer through early diagnosis, secondary prevention and the formulation of individualised treatment plans. The condition is managed through various treatment options such as medical and surgical therapy performed either in-house or in collaboration with other specialties and coordinating follow-up arrangements. The Clinic also functions as an information resource for patients and their caregivers as well as a platform to enhance training of doctors. The Skin Cancer Clinic operates every Thursday.
Clinical Indicator:
Rate of Incomplete Tumor Excision
Urticaria and Angioedema Clinic
Consultant-in-charge: Dr Tee Shang-Ian
Urticaria and Angioedema Clinic aims to improve the accuracy of diagnosis and treatment of urticaria and angioedema, establish a national database for basic and clinical research in this field in order to function as an information resource for affected patients and their care givers, while enhancing the training for doctors. This clinic provides physical and skin testing / challenge testing facilities, where patients with urticaria and angioedema receive in-depth diagnosis and assessment and are advised on allergen/ additive avoidance.
Wound and Ulcer Clinic
Associate Consultant-in-charge: Dr Michelle Liang
The aim of the Wound and Ulcer Clinic is to provide specialist assessment, diagnosis and management of chronic wounds and ulcers. A wide variety of ulcers are seen at this clinic, including venous leg ulcers, diabetic ulcers, vasculitic ulcers and chronic wounds of unknown etiology for diagnostic work-up. Wound management provided includes basic dressings, surgical debridement, compression bandaging and advanced dressings. Appropriate referrals to other specialists will be coordinated to ensure a multi-disciplinary approach to optimise wound healing.