The blood supply of the leg consists of blood vessels called veins that return blood from the lower legs to the heart, assisted by valves that ensure that the “one-way” upward flow of blood. In many patients with venous leg ulcers, these valves are not working properly, causing blood to “pool” in the lower legs. This can lead to swelling and darkening of the skin, and eventually to venous leg ulcers (Figure 4).
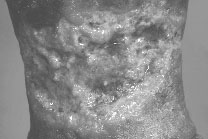
Fig 4 Venous Leg Ulcer - The skin of the leg can turn dark brown or red.
The ulcer is usually wet and weepy, with heavy discharge.